There are three main types of ticks that infect domestic animals in Australia – paralysis ticks, bush ticks and brown dog ticks. The most harmful is Ixodes holocyclus – the paralysis tick. Famously known for its debilitating toxin that can be fatal to any of our dogs and cats at any stage in their life.
The threat of these ticks were traditionally seasonal, with increasing numbers found between September and March – however, due to environmental changes such as global warming, pet owners should exercise caution all year round. Wild animals such as possums, bandicoots and rats can also act as ‘vectors’ for ticks – meaning they are immune to to their toxins, and instead act as transportation for ticks to spread into our backyards and homes. The ticks fall off the coat of the
wild animal as it roams through the neighbourhoods.
What does a paralysis tick look like?
A paralysis tick can take on different forms depending on its maturation, however is usually only found in its fully engorged state when attached to an animal.
See Figure 1. depicting the different types of common ticks found on the East Coast. Note that the ‘nymph’ (baby) stages of these ticks all look very similar. To help distinguish a paralysis tick, their legs are found close to the head region, and alternate in colour between brown and white.
If unsure, it’s always better to consult with a Veterinary professional. The tick needs to be removed regardless, as even the less harmful bush/brown dog ticks can cause localised irritation and transmit other infectious diseases (such as babesiosis).
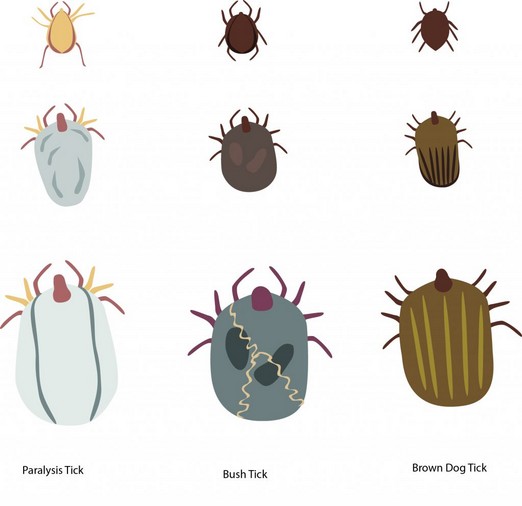
Figure 1. Tick life stages (Sash Vets, 2022)
Why are paralysis ticks so dangerous?
While a paralysis tick is attached to an animal, it feeds on the blood. While it does this, toxins are released into the blood stream. The toxin that paralysis ticks secrete targets the connection between the nerves and muscles of the body – hence causing paralysis, as in the name. As the paralysis progresses, it can interfere with major muscles used for breathing, swallowing and heart contraction. If left untreated, the animal can succumb to aspiration pneumonia, asphyxiation, or even cardiac arrest.
I have found a tick on my pet. What do I do?
It is always better to remove the tick – no matter the type – immediately from your animal. Ticks prefer hot, moist areas so if you’re on the hunt, move your fingertips through the fur at skin level. Any lump or bump you can feel needs to be looked at in case a tick is attached. Start at the head (including inside the mouth and ears), down the legs (including in between the toes/paw pads), and finish at the tail (including around the anus and genital folds).
If a tick is identified, remove it by pinching the skin around the tick with your non-dominant hand. With your dominant hand, use your thumb and index fingers to grab the tick as close to the head as possible. Firmly pull the tick out of the skin. Tick twisters can assist with this if needed, and can be purchased at our clinic or any major pet store. Place the tick into a vessel for the Veterinarian to identify. (Don’t be worried if the head isn’t fully removed as well – this poses no harm to the pet if left in, and can be removed later)
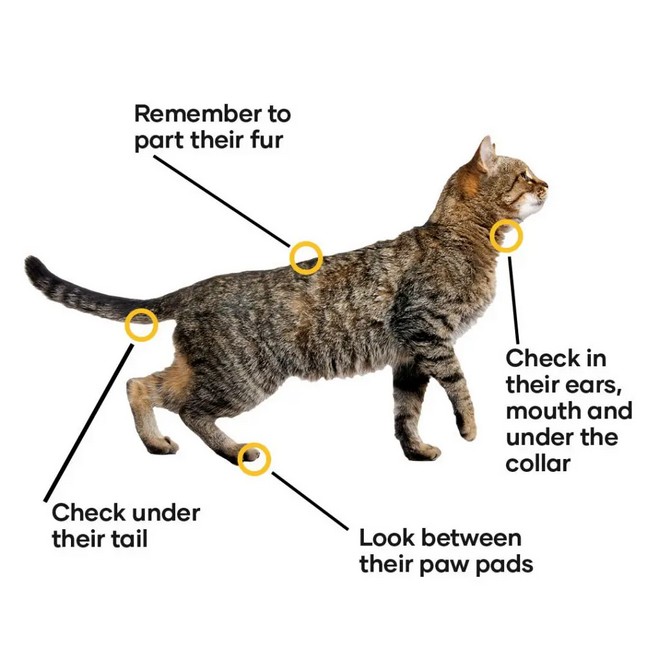
Figure 2: Common locations tick are found on an animal (PetBarn, 2020)
If your pet is affected by tick paralysis, there is still hope – symptoms can be reversed. Here at Morayfield Vet Clinic, we have implemented our own tick paralysis treatment protocol. This involves using ‘tick anti-serum’, which is administered during their stay. Keep in mind, full recovery largely depends on the combined effort of early identification/removal and tick anti-serum treatment. Even if your pet is suffering from mild symptoms, it is best to seek intervention immediately to improve the chances of recovery.
Tick paralysis symptoms
Sometimes, pet owners may not be aware their animal has a tick attached to them until symptoms show. If your pet is exhibiting any of the following, phone the clinic immediately and a nurse will be able to triage you. Keep in mind even the mildest of symptoms are treated as serious – there is a high chance the condition will worsen, even if the tick is found and removed early on.
- Wobbly legs, especially hind limbs
- Change in bark/meow
- Vomiting, gagging, retching, trouble swallowing food/water
- Dilated pupils
- Salivation/respiratory noise
- Difficulty breathing
- Leaking urine or faeces
- Collapse

Figure 3: Tick paralysis treatment (The Conversation, 2016)
What can I expect if my pet undergoes tick paralysis treatment?
Once tick paralysis treatment has been indicated, the Vet will guide you through the expectations during and after treatment. The following outlines some of the procedures our staff will perform during your pet’s stay (unless otherwise discussed):-
- frequent TPR checks by our intensive care nursing team
- sedation (to lessen anxiety/stress)
- symptomatic treatment e.g. manual heating, bladder expression and passive movement
- tick anti-serum administration (to lessen the effects of the tick paralysis toxin
- intravenous fluids (to maintain appropriate blood pressure which helps filter medications)
- medication administration e.g. antibiotics and anti-emetics
- Bravecto spot on application (to kill other ticks on the body that haven’t been found yet)
- full body clip (to make sure no other ticks are attached)
Recovery even after the pet receives tick anti-serum is not instantaneous. It takes time for the tick paralysis toxin to be completely filtered out of the blood stream, and symptoms can persist for a few days (even up to a week) afterwards, and clinical deterioration can still occur post treatment. This is where referral to emergency specialists are sometimes required. Pet owners need to bare in mind that referral to a Vet specialist centre (such as BVSC or QVS) is needed if:-
- symptoms are severe enough that manual ventilation/oxygen therapy is required
- the patient presents late in the day and there is not enough time to follow out full treatment
- we do not have the capacity to offer gold standard of care for any reason
- the patient needs overnight observation after tick paralysis treatment at our clinic
- the patient continues to deteriorate despite tick anti-serum treatment
Prevention
Tick paralysis can be almost entirely prevented through the form of prophylactics. Common products such as NexGard Spectra, Bravecto, Simparica and Revolution Plus can be purchased at our clinic or any major pet store, usually in form of a chewable tablet or spot-on treatment. Please keep in mind Vet recommended tick preventatives are only sold at Vet clinics. Keeping your pet up to date with products like this is critical in not only keeping them safe from ticks, but also in maintaining their overall health.
Call the clinic today if you have any further queries regarding this topic!
Resources
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4084664/
https://sashvets.com/pet-advice/tick-paralysis/
https://www.akc.org/expert-advice/health/how-to-remove-tick-from-dog/
https://www.greencrossvets.com.au/pet-library/articles-of-interest/get-ticked-off/
https://www.petbarn.com.au/petspot/cat/medical-vet-services-cat/protect-your-pets-against-tickparalysis/
https://theconversation.com/ticked-off-lets-stop-our-dogs-and-cats-dying-of-tick-paralysis-thisyear-63383
